Introduction
In contemporary medical practice, the most crucial criterion for treatment success is the restoration of the anatomical form and functional value of the affected organ or system [1, 2]. A significant challenge for dental practitioners is the restoration of proximal surfaces on lateral teeth, as the operative treatment of carious lesions focuses on reestablishing the anatomical and physiological characteristics of interproximal relationships.
The interproximal relationship is defined as the correlation between neighboring teeth of the same dental arch or the relationship that exists between the mesial surface of one tooth and the distal surface of the adjacent tooth. As a fundamental element of the interproximal assembly, the restoration of the interdental contact results from understanding its functionality. It is defined as the location where the maximum prominence area of the mesial or distal contour of a tooth contacts its adjacent counterpart in the same arch [3, 4]. Studies have found that the interproximal contact established by intact natural teeth takes the form of a point in individuals up to 20 years old; in individuals aged 20-40 years it is represented by a surface area of 1.5 mm2; and in individuals over 40 years old, it reaches a surface area of 4.5 mm2 [5]. This is due to physiological dental movements during the masticatory process that generate friction between neighboring teeth at their contact point, transforming the point into a more or less extended surface, which is determined by the direction and axis of movements. In the case of lateral teeth, the predominant axis is transversal, resulting in movements towards the free surfaces. Physiological mobility is higher in erupting teeth, in women compared to men, in children compared to adults, and is lower in teeth without antagonists or those with severe attrition. Measurements taken in individuals aged 45-50 years with a healthy oral cavity and complete dentition have shown 10 mm of enamel abrasion from the contact areas of teeth in one arch. This is approximately 0.38 mm per contact area of each tooth [4, 6]. Thus, in older individuals, the contact area has a larger and flatter surface [7].
Anatomically, the contact surface is located at the level of the maximum contour of the proximal surfaces. For lateral teeth, it is positioned at the transition between the middle and occlusal third of the cervico-occlusal distance and at the transition between the middle and buccal third of the buccal-oral distance [8]. Some studies have found that the size, location, and shape of contact areas also depend on the anatomical contours and convergence of proximal surfaces, respectively, the mesial or distal placement [9].
The importance of properly restoring the interdental contact is determined by the series of its functions:
stabilizes the position of the teeth, facilitating the transmission of masticatory forces;
maintains the integrity of the dental arch;
prevents food impaction, which in turn can cause masticatory discomfort, recurrent dental caries, periodontal disease, or lead to dental migration;
protects the interdental papilla by diverting food towards the buccal and oral direction, preventing trauma and inflammation [4, 7, 10].
Alongside anatomical positioning, an essential criterion is the tightness of interdental contact. A sufficiently tight proximal contact resists separation forces during mastication and prevents food impaction. Lack of contact or insufficient tightness is associated with periodontal disease, tooth tilting, disturbance of occlusal relationships with antagonists, and retention of bacterial plaque in the interproximal space [11].
Thus, the cornerstone in interdental contact management is adhering to the biomimetic concept, which involves restoring of the damaged portions of the tooth according to the natural tooth's characteristics regarding appearance, biomechanical competencies, and function [12].
The purpose of the study was to radiologically evaluate the proximal morphology of restored surfaces on lateral teeth and the positioning of interdental contact.
Material and methods
The study included 100 digital bite-wing radiographs, which according to the literature, are the most effective for the diagnosis of proximal lesions on lateral teeth, the assessment of qualitative parameters of proximal restorations, as well as the positioning of the contact area. Bite-wing radiographs were selected based on the presence of proximal restorations on lateral teeth which were related to a neighboring tooth, marking an interproximal area. They included the I premolar – II molar area and were taken over the course of one year.
The restorations were analyzed according to their location:
at the level of molars or premolars;
in the upper or lower arch;
on the mesial or distal surface.
The proximal morphology of the restorations was evaluated by assessing the emergence profile categorized as concave, convex, or straight surface. Similarly, the cervical marginal adaptation of the restoration was studied by evaluating the presence of a harmonious transition between tooth and restoration or a visible radiographic overhang (Fig. 1), with the calculation of its size.
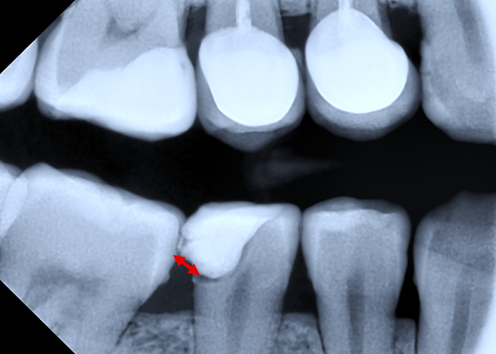 |
Fig. 1 Bitewing radiography. Distal restoration in tooth 45 with the presence of overhang. Note: Red line – overhang. |
The adjacent tooth to the restoration was assessed as:
intact tooth without proximal cavity lesion (Fig. 2);
tooth with proximal restoration (the emergence profile of the restoration was determined) (Fig. 3);
tooth with crown coverage (the emergence profile of the crown was determined).
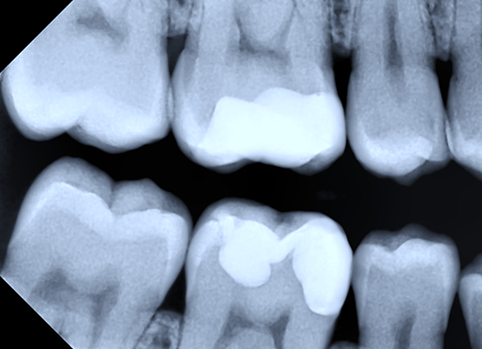 |
Fig. 2 Bitewing radiography. Mesial restoration (convex emergence profile) in tooth 16 with intact adjacent tooth. Mesial restoration (convex emergence profile) in tooth 46 with intact adjacent tooth. |
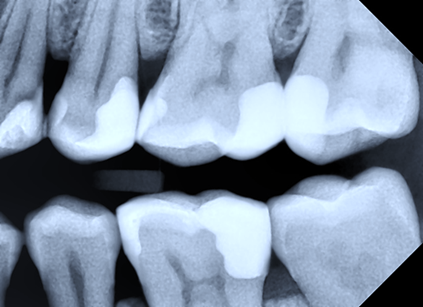 |
Fig. 3 Bitewing radiography. Distal restorations in teeth 24, 25, 26 with adjacent teeth with proximal restorations. |
Subsequently, the interdental contact was analyzed by evaluating its presence or absence (Fig. 4), as well as its positioning in the cervico-occlusal direction, with the establishment of anatomical or non-anatomical localization.
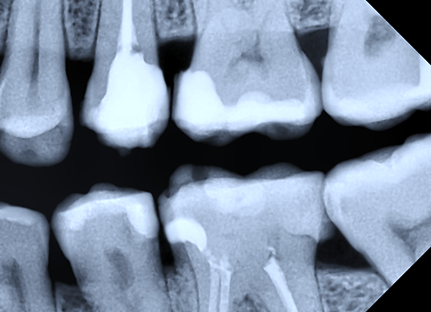 |
Fig. 4 Bitewing radiography. Proximal restorations with the absence of interdental contact between teeth 25-26, 35-36. |
For lateral teeth, where the contact area is anatomically positioned at the maximum contour of the proximal surfaces and at the transition between the middle and occlusal third of the cervico-occlusal distance, three distances were calculated (Fig. 5):
distance between adjacent teeth at the cemento-enamel junction (CEJ);
distance from the CEJ to the middle of the contact area;
distance from the CEJ to the occlusal edge, along the cervico-occlusal distance.
To calculate the middle of the cervico-occlusal distance, the following formula was applied:
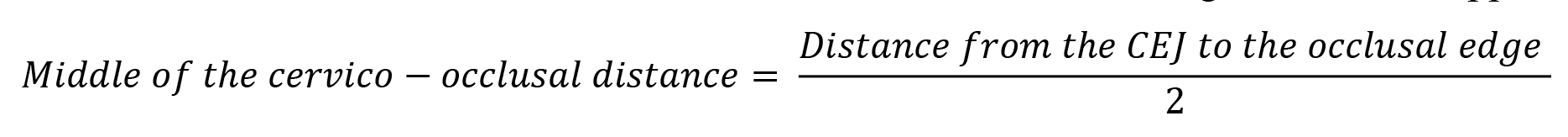
To calculate the occlusal third of the cervico-occlusal distance, the following formula was applied: 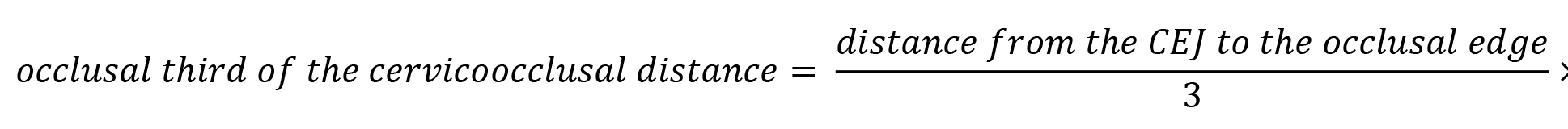
Thus, the anatomical positioning of the interdental contact was considered to fall within the interval between the point representing the middle of the cervico-occlusal distance and the point representing 2/3 of the cervico-occlusal distance, calculated from the cervical level.
The obtained data were subjected to statistical evaluation with the software Epi Info 7.2 and Microsoft Excel 2019 in order to establish statistical differences in the sample studied. For this, a95% confidence interval was calculated. A significant level (p-value) of 0.05 was set to indicate whether the observed differences were statistically significant.
 |
Fig.5 Bitewing radiography. Distances measurements. Note: Blue line - distance between adjacent teeth at the cemento-enamel junction (CEJ). Yellow line - distance from the CEJ to the middle of the contact area. Red line - distance from the CEJ to the occlusal edge, along the cervico-occlusal distance. |
Results
By analyzing the proximal restorations' location based on the obtained data from 100 bite-wing radiographies, the following results were obtained.
Analysis of proximal restorations regarding their location. Table 1 shows the data at the level of molars or premolars.
Table 1. Location of restoration according to tooth type. | ||||
Molar or premolar | Abs. | Percent | Exact 95% LCL | Exact 95% UCL |
Molar | 42 | 42,0 % | 32,2 % | 52,3 % |
Premolar | 58 | 58,0 % | 47,7 % | 67,8 % |
TOTAL | 100 | 100,00 % | ||
Note: Abs – absolute value; LCL – Lower Confidence Limit; UCL – Upper Confidence Limit. Statistical evaluation was performed with the software Epi Info 7.2. Descriptive analysis was provided. Confidence Interval (CI) – 95% was calculated. A significant level (p-value) of 0.05 was considered statistically significant. | ||||
The table provides data on the distribution of restorations at the level of molars and premolars in a sample, where restorations at the molar level represent 42.0% (95% CI: 32.2-52.3) of the total 100 observations, while restorations at the premolar level are present in 58.0% (95% CI: 47.7-67.8) of cases.
By comparing the confidence intervals, it can be assessed if there is a statistically significant difference between the proportions of restorations at the molar and premolar levels. In this case, the two 95% confidence intervals overlap, indicating that there is no significant difference between the frequency of restorations at the molar and premolar levels in the sample studied (p>0.05). Table 2 demonstrates the data at the level of the upper or lower arch.
Table 2. Location of restoration according to the dental arch. | ||||
Upper or lower dental arch | Abs. | Percent | Exact 95% LCL | Exact 95% UCL |
Upper dental arch | 61 | 61,0 % | 50,7 % | 70,6 % |
Lower dental arch | 39 | 39,0 % | 29,4 % | 49,3 % |
TOTAL | 100 | 100,00 % | ||
Note: Abs – absolute value; LCL – Lower Confidence Limit; UCL – Upper Confidence Limit. Statistical evaluation was performed with the software Epi Info 7.2. Descriptive analysis was provided. Confidence Interval (CI) – 95% was calculated. A significant level (p-value) of 0.05 was considered statistically significant. | ||||
The table provides data on the distribution of restorations in the upper or lower arch in a sample, where restorations in the upper arch represent 61.0% (95% CI: 50.7-70.6) of the total 100 observations, while restorations in the lower arch are present in 39.0% (95% CI: 29.4-49.3) of the cases. In this case, the two intervals do not overlap, indicating a difference (p < 0.05) between the frequency of restorations in the upper and lower arches in the studied sample. Table 3 represents the data at the level of mesial or distal surface.
Table 3. Location of restoration according to the proximal surface of the tooth | ||||
Mesial or distal surface | Abs. | Percent | Exact 95% LCL | Exact 95% UCL |
Mesial surface | 40 | 40,0 % | 30,3 % | 50,3 % |
Distal surface | 60 | 60,0 % | 49,7 % | 69,7 % |
TOTAL | 100 | 100,00 % | ||
Note: Abs – absolute value; LCL – Lower Confidence Limit; UCL – Upper Confidence Limit. Statistical evaluation was performed with the software Epi Info 7.2. Descriptive analysis was provided. Confidence Interval (CI) – 95% was calculated. A significant level (p-value) of 0.05 was considered statistically significant | ||||
The table presents the distribution of restorations based on the location on the mesial or distal surface of the tooth in a sample studied. Restorations on the mesial surface of the tooth constitute 40.0% (95% CI: 30.3-50.3) of the total 100 observations, while restorations on the distal surface represent 60.0% (95% CI: 49.7-69.7). In this context, the fact that the two intervals almost do not overlap suggests an insignificant difference in the frequency of restoration localization on the mesial or distal surfaces in the studied sample.
Table 4. Emergence profile of the restored surface. | ||||
Convex, concave or straight | Abs. | Percent | Exact 95% LCL | Exact 95% UCL |
Convex | 71 | 71,0 % | 61,1 % | 79,6 % |
Concave | 3 | 3,0 % | 0,6 % | 8,5 % |
Straight | 26 | 26,0 % | 17,7 % | 35,7 % |
TOTAL | 100 | 100,00 % | ||
Note: Abs – absolute value; LCL – Lower Confidence Limit; UCL – Upper Confidence Limit. Statistical evaluation was performed with the software Epi Info 7.2. Descriptive analysis was provided. Confidence Interval (CI) – 95% was calculated. A significant level (p-value) of 0.05 was considered statistically significant. | ||||
Table 4 provides the distribution of convex, concave, and straight emergence profiles of the restored surface in a studied sample. Out of a total of 100 observations, the convex emergence profile is the most common, representing 71.0% (95% CI: 61.1-79.6), followed by the straight emergence profile at 26.0% (95% CI: 17.7-35.7), and the concave emergence profile at 3.0% (95% CI: 0.6-8.5). In this case, the three confidence intervals do not completely overlap, indicating a possible significant difference in the frequency of these profiles in the studied sample (p < 0.05).
This suggests that the convex emergence profile of the restored surface is the most commonly encountered, while the concave emergence profile is the least encountered. However, to confirm these observations and assess the statistical significance of the observed differences, it is advisable to use additional statistical methods such as hypothesis testing or regression analysis.
Table 5. Cervical marginal adaptation of the proximal restoration. | ||||
Adapted, overhang, invagination | Abs. | Percent | Exact 95% LCL | Exact 95% UCL |
A | 66 | 66,0 % | 55,8 % | 75,2 % |
I (0,4) | 1 | 1,0 % | 0,0 % | 5,4 % |
O (0,1) | 3 | 3,0 % | 0,6 % | 8,5 % |
O (0,2) | 4 | 4,0 % | 1,1 % | 9,9 % |
O (0,3) | 6 | 6,0 % | 2,2 % | 12,6 % |
O (0,4) | 5 | 5,0 % | 1,6 % | 11,3 % |
O (0,5) | 5 | 5,0 % | 1,6 % | 11,3 % |
O (0,6) | 4 | 4,0 % | 1,1 % | 9,9 % |
O (0,7) | 1 | 1,0 % | 0,0 % | 5,4 % |
O (0,8) | 1 | 1,0 % | 0,0 % | 5,4 % |
O (0,9) | 3 | 3,0 % | 0,6 % | 8,5 % |
O (1,1) | 1 | 1,0 % | 0,0 % | 5,4 % |
TOTAL | 100 | 100,00 % | ||
Note: A - adapted, O - overhang, I – invagination; Abs – absolute value; LCL – Lower Confidence Limit; UCL – Upper Confidence Limit. Statistical evaluation was performed with the software Epi Info 7.2. Descriptive analysis was provided. Confidence Interval (CI) – 95% was calculated. A significant level (p-value) of 0.05 was considered statistically significant. | ||||
Table 5 provides the distribution of cervical marginal adaptations of proximal restorations in a studied sample, where "A" represents harmonious adaptation, "O" represents the presence of an overhang, and "I" represents the presence of an invagination at the cervical level.
Out of a total of 100 observations, harmonious adaptation "A" is the most commonly encountered, representing 66.0% (95% CI: 55.8-75.2). The presence of invagination "I" and the presence of an overhang "O" are less frequent, representing 1.0% (95% CI: 0.0-5.4) and 3.0% (95% CI: 0.6-8.5) respectively.
The difference between the observed frequencies suggests that harmonious cervical marginal adaptation of the restoration is predominant (p < 0.05) compared to the other two types of adaptation. However, 34% of cases show a non-harmonious cervical marginal adaptation, represented by an overhang or invagination.
Table 6. Adjacent tooth to the restored proximal surface. | ||||
Intact, restoration, crown | Abs. | Percent | Exact 95% LCL | Exact 95% UCL |
In | 35 | 35,0 % | 25,7 % | 45,2 % |
R | 61 | 61,0 % | 50,7 % | 70,6 % |
Co | 4 | 4,0 % | 1,1 % | 9,9 % |
TOTAL | 100 | 100,00 % | ||
Note: In - intact, R - restoration, Co - crown; Abs – absolute value; LCL – Lower Confidence Limit; UCL – Upper Confidence Limit. Statistical evaluation was performed with the software Epi Info 7.2. Descriptive analysis was provided. Confidence Interval (CI) – 95% was calculated. A significant level (p-value) of 0.05 was considered statistically significant. | ||||
Table 6 provides the distribution of the adjacent tooth's condition to the restored proximal surface, which can be intact "In", restored "R", or having a crown "Co", in a studied sample.
Out of a total of 100 observations, it is underlined that the majority of adjacent teeth are restored, representing 61.0% (95% CI: 50.7-70.6). The intact adjacent tooth constitutes 35.0% (95% CI: 25.7-45.2), while the presence of a crown is observed in 4.0% (95% CI: 1.1-9.9) of cases. This distribution suggests that the restored adjacent tooth is the most commonly encountered (p < 0.05) among the adjacent teeth, followed by the intact adjacent tooth and the one with a crown.
Table 7. Emergence profile of the adjacent tooth surface (convex, concave, straight). | ||||
Adjacent tooth surface convex, concave, straight | Abs. | Percent | Exact 95% LCL | Exact 95% UCL |
Convex | 84 | 84,0 % | 75,3 % | 90,6 % |
Straight | 16 | 16,0 % | 9,4 % | 24,7 % |
TOTAL | 100 | 100,00 % | ||
Note: Abs – absolute value; LCL – Lower Confidence Limit; UCL – Upper Confidence Limit. Statistical evaluation was performed with the software Epi Info 7.2. Descriptive analysis was provided. Confidence Interval (CI) – 95% was calculated. A significant level (p-value) of 0.05 was considered statistically significant. | ||||
Table 7 provides data on the distribution of the emergence profile of the adjacent tooth surface in a specific sample, classifying the surfaces as convex, concave, or straight. Out of a total of 100 observations, it can be noted that the surfaces of the adjacent tooth are predominantly convex, representing 84.0% (95% CI: 75.3-90.6) of the total. In contrast, straight surfaces are recorded in a smaller proportion, accounting for only 16.0% (95% CI: 9.4-24.7), while concave surfaces are absent.
These findings indicate that convex surfaces are the most common (p < 0.05) among the adjacent teeth, suggesting a predominant trend towards this shape. At the same time, straight surfaces are less common in this sample.
Table 8. Interdental contact (presence, absence). | ||||
Presence, absence of interdental contact | Abs. | Percent | Exact 95% LCL | Exact 95% UCL |
Presence | 81 | 81,0 % | 71,9 % | 88,2 % |
Absence | 19 | 19,0 % | 11,8 % | 28,1 % |
TOTAL | 100 | 100,00 % | ||
Note: Abs – absolute value; LCL – Lower Confidence Limit; UCL – Upper Confidence Limit. Statistical evaluation was performed with the software Epi Info 7.2. Descriptive analysis was provided. Confidence Interval (CI) – 95% was calculated. A significant level (p-value) of 0.05 was considered statistically significant. | ||||
Table 8 presents the distribution of interdental contact in a studied sample, categorizing the contact as either "present" or "absent". Out of a total of 100 observations, it is observed that the majority of interproximal relationships have interdental contacts, representing 81.0% (95% CI: 71.9-88.2). In contrast, the absence of interdental contact is observed in 19.0% (95% CI: 11.8-28.1) of cases.
These findings suggest that in the majority of cases, there is interdental contact (p < 0.05). However, it is important to note that approximately one-fifth of cases exhibit the absence of the contact.
Table 9. Distance between adjacent teeth at the CEJ. | |||||
Distance, mm | Abs. | Percent | Exact 95% LCL |
| Exact 95% UCL |
0,5-1 | 3 | 3,0 % | 0,6 % |
| 8,5 % |
1,1-1,5 | 18 | 18,0 % | 11,0 % |
| 26,9 % |
1,6-2,0 | 42 | 42,0 % | 32,2 % |
| 52,3 % |
2,1-2,5 | 31 | 31,0 % | 22,1 % |
| 41,0 % |
2,6-3,0 | 3 | 3,0 % | 0,6 % |
| 8,5 % |
> 3 | 3 | 3,0 % | 0,6 % |
| 8,5 % |
TOTAL | 100 | 100,00 % |
| ||
Note: CEJ – cemento-enamel junction; Abs – absolute value; LCL – Lower Confidence Limit; UCL – Upper Confidence Limit. Statistical evaluation was performed with the software Epi Info 7.2. Descriptive analysis was provided. Confidence Interval (CI) – 95% was calculated. A significant level (p-value) of 0.05 was considered statistically significant. | |||||
Table 9 provides information on the distribution of the distance between adjacent teeth at the cemento-enamel junction (CEJ). The distance is divided into intervals to allow for a more detailed analysis of the distribution of these measurements.
Out of the 100 recorded observations, it can be emphasized that the intervals 1.6-2.0 and 2.1-2.5 dominate the distribution, representing 42.0% (95% CI: 32.2-52.3) and 31.0% (95% CI: 22.1-41.0) of the total sample, respectively. This suggests that the majority of distances between adjacent teeth at the CEJ fall within these intervals.
Additionally, it can be noticed that smaller intervals, such as 0.5-1 and 1.1-1.5, represent lower percentages of the total sample, indicating that smaller distances are less common in this study. The intervals represent 3.0% (95% CI: 0.6-8.5) and 18.0% (95% CI: 11.0-26.9) of the sample, respectively.
Regarding larger values, from 2.6-3.0 and above 3, these are less frequently encountered, each representing 3.0% (95% CI: 0.6-8.5) of the sample. This may suggest the presence of some exceptional cases where the distance between teeth is greater.
Table 10. Mean and median of the distance between adjacent teeth at the CEJ. | ||||||
Obs | Mean | Std Dev | Min | Median | Max | |
Distance between adjacent teeth at the level of CEJ | 100 | 1,8 | 0,5 | 0,8 | 1,8 | 4,4 |
Note: CEJ – cemento-enamel junction; Abs – absolute value; LCL – Lower Confidence Limit; UCL – Upper Confidence Limit. Statistical evaluation was performed with the software Epi Info 7.2. Descriptive analysis was provided. Confidence Interval (CI) – 95% was calculated. A significant level (p-value) of 0.05 was considered statistically significant. | ||||||
These data provide insight into the distribution of the distance between adjacent teeth at the CEJ within the sample studied. The mean distance between adjacent teeth at the CEJ is approximately 1.8 mm, with a standard deviation of 0.5, indicating that the majority of observations clusters are around mean value, with moderate dispersion. There is significant variation in the distance between adjacent teeth within the sample, with a minimum recorded value of 0.8 and a maximum value of 4.4. This variation demonstrates significant differences in tooth spacing among the analyzed cases.
The median distance between teeth at the CEJ is 1.8, indicating that half of the observations have a distance less than or equal to 1.8, while the other half have a distance greater than or equal to 1.8. This highlights a relatively balanced distribution of data around the median.
Table 11. Positioning of the interdental contact (anatomical, non-anatomical). | ||||
Anatomical, non-anatomical | Abs. | Percent | Exact 95% LCL | Exact 95% UCL |
Anatomical | 28 | 34,6 % | 24,3 % | 46,0 % |
Non-anatomical | 53 | 65,4 % | 54,0 % | 75,7 % |
TOTAL | 81 | 100,00 % | ||
Note: Abs – absolute value; LCL – Lower Confidence Limit; UCL – Upper Confidence Limit. Statistical evaluation was performed with the software Epi Info 7.2. Descriptive analysis was provided. Confidence Interval (CI) – 95% was calculated. A significant level (p-value) of 0.05 was considered statistically significant. | ||||
The table presents the distribution of the positioning of the interdental contact within the studied sample, classified into anatomical and non-anatomical. In this category, anatomical positioning accounts for 35.0% (95% CI: 24.7-46.5) out of a total of 81 observations, indicating that approximately one-third of dental contacts are considered anatomically positioned. The distribution (p < 0.05) is dominated by non-anatomical positioning which represents 65.0% (95% CI: 53.5-75.3) of the total sample. This suggests that the majority of dental contacts are positioned in a manner considered non-anatomical.
Discussion
Reproducing an anatomical proximal contour represents a primary objective in proximal restorations and is crucial for maintaining the health of the underlying periodontal tissues [13]. Similarly, it minimizes the risk of recurrent caries as a complex multifactorial process that requires careful analysis of the restoration, along with the chemical and bacterial effects of the oral environment [14].
The results of the study showed that restorations at the level of lateral teeth are more commonly encountered in the upper dental arch than in the lower one and on distal surfaces more than mesial ones. The increased frequency of carious lesions in the upper teeth underlines the necessity for restorative treatment. This finding may be influenced by the reduced visibility of teeth in the upper arch by the patient, leading to late detection of carious processes and delayed referral to the dentist for treatment. The prevalence on distal surfaces is determined by poorer oral hygiene in this region, with difficulties in using adjunctive oral hygiene aids such as floss and interdental brushes. This increases the risk of bacterial plaque accumulation, which is the determining factor in the onset of carious process.
Regarding the evaluation of the emergence profile of the restored surfaces, a predominance of the convex profile, considered anatomical, was observed. However, a fairly high percentage of straight and concave profiles, classified as non-anatomical, were also evident. This leads to the difficulty of achieving an anatomical interdental contact, which according to the definition is formed by the maximum proximal prominence areas of the adjacent teeth.
The cervical marginal adaptation of restorations may present either a harmonious transition between the tooth and the restoration or the presence of an invagination and cervical overhang. These irregularities represent plaque retention areas, making oral hygiene challenging and potentially leading to restoration displacement, jeopardizing the success of restorative treatment and its maintenance over time. Mjor et al. reported that the gingival wall of the proximal restoration on lateral teeth is the most common site of recurrent caries [15-17].
The data obtained in the current study are consistent with those reported in a previous cross-sectional study, which highlighted that one-third of the analyzed proximal restorations had secondary marginal overhangs [18]. The occurrence of such areas of unsatisfactory marginal adaptation is conditioned by factors centered on the dentist, revealing gaps in following the principles of proximal surface restoration in lateral teeth, including the inappropriate use of matrices, interdental wedges, and separation rings depending on the present clinical situation.
As a result of obtaining a deficient emergence profile and unsatisfactory marginal adaptation, cases of missing interdental contact were noted. However, its presence prevails in the conducted study, indicating that even in the case of a deficient emergence profile, an interdental contact can be achieved. Nevertheless, it is essential to evaluate the contact’s tightness, which is much more important than its mere presence. Studies have concluded that the presence and tightness of the interdental contact are determined by the type of restored tooth, its location, the time of day when it was restored, the periodontal status of the tooth, and manifest a high degree of individual variability [8].
Similarly, the positioning of the contact area plays an essential role in performing its functions. The respective study found that in the majority of cases, the interdental contact was present, but it corresponded to a non-anatomical positioning, which prevailed over the anatomical one. This finding may also be influenced by the distance between adjacent teeth at the CEJ, so that a greater distance requires the use of special anatomical sectional matrices with larger curvatures, which are not possessed by every practitioner. Thus, the distance influences the presence of the interdental contact and its anatomical positioning.
Conclusions
The radiological assessment of proximal restorations on lateral teeth and of interdental contacts found that they do not always meet anatomical requirements and fail to fulfill all qualitative parameters. Concave and straight emergence profiles of restorations, the presence of invaginations and overhangs at the cervical level, absence of interdental contact, or its non-anatomical positioning indicate the necessity to revise the principles of restoring proximal surfaces on lateral teeth, by using accessories to restore the interproximal relationship according to the clinical situation.
Competing interest
None declared.
Authors’ contributions
VA performed the study, drafted the first manuscript and interpreted the data; DM completed the final text, and SC revised the manuscript. All the authors approved the final version of the manuscript.
Funding
The study was the authors’ initiative. The authors are independent and take responsibility for the integrity of the data and accuracy of the data analysis.
Patient consent
Obtained.
Ethics approval
The study was done within the doctoral program whose research project was approved by the Committee of Research Ethics with number 1 on 12.11.2021.
Provenance and peer review
Not commissioned, externally peer review.
Authors’ ORCID IDs
Victoria Ababii – https://orcid.org/0000-0001-9827-2239
Diana Marcu – https://orcid.org/0000-0002-3844-9175
Sergiu Ciobanu – https://orcid.org/0000-0002-7955-545x
References
Coulehan JL, Block ML. The medical interview: mastering skills for clinical practice. 5th ed. Philadelphia: Davis Company, 2005. 409 p.
Vedeneva EV, Gurevich KG, Vagner VD, Fabricant EG. Sviazi klinicheskoi kartiny i kachestva zhizni patsientov obrashchaiushchikhsia za esteticheskim stomatologicheskim lecheniem [Relationship between the clinical picture and quality of life of patients seeking aesthetic dental treatment]. Stomatologiia dlia Vsekh. 2009;(4):4-6. Russian.
Peumans M, Venuti P, Politano G, Van Meerbeek B. Effective protocol for daily high-quality direct posterior composite restorations. The interdental anatomy of the class-2 composite restoration. J Adhes Dent. 2021;23(1):21-34. doi: 10.3290/j.jad.b916819.
Roberson TM, Heymann HO, Swift EJ Jr., editors. Sturdevant’s art and science of operative dentistry. 5th ed. St. Louis: Mosby Elsevier; 2006. 1006 p. ISBN 978-0-323-03009-0.
Nikolaev AI, Ginali AN, Permiakova AV, Shashmurina VR. Karta localizatsii kontaktnykh punktov i kontaktnykh ploshchadok bokovykh zubov [Reference map of localization of contact points and contact areas of posterior teeth]. Meditsinskii Alfavit. 2021;(4):34-38. Russian. doi: 10.33667/2078-5631-2021-24-34-38.
Figún ME, Garino RR. Anatomía odontológica: functional y aplicada [Functional and applied dental anatomy]. 2nd ed. Buenos Aires: El Ateneo; 2001. 520 p. ISBN 950-02-0125-9. Spanish.
Scheid RC, Weiss G. Woelfel’s dental anatomy. 8th ed. Philadelphia: Wolters Kluwer/Lippincott Williams and Wilkins; 2012. 504 p.
Dörfer CE, von Bethlenfalvy ER, Staehle HJ, Pioch T. Factors influencing proximal dental contact strengths. Eur J Oral Sci. 2000 Oct;108(5):368-77. doi: 10.1034/j.1600-0722.2000.108005368.x.
Woelfel JB, Scheid RC. Anatomía dental: aplicaciones clínicas [Dental anatomy: clinical applications]. Barcelona: Masson Williams & Wilkins; 1998. 498 p. ISBN 84-8315-007-7. Spanish.
Bailey O. Sectional matrix solutions: the distorted truth. Br Dent J. 2021 Nov;231(9):547-555. doi: 10.1038/s41415-021-3608-5.
Peumans M, Van Meerbeek B, Asscherickx K, Simon S, Abe Y, Lambrechts P, Vanherle G. Do condensable composites help to achieve better proximal contacts? Dent Mater. 2001 Nov;17(6):533-41. doi: 10.1016/s0109-5641(01)00015-x.
Zafar MS, Amin F, Fareed MA, et al. Biomimetic aspects of restorative dentistry biomaterials. Biomimetics (Basel). 2020;5(3):34. doi: 10.3390/biomimetics5030034.
Kampouropgoulos D, Paximada C, Loukidis M, Kakaboura A. The influence of matrix type on the proximal contact in Class II resin composite restorations. Oper Dent. 2010 Jul-Aug;35(4):454-62. doi: 10.2341/09-272-L.
Elgezawi M, Haridy R, Abdalla MA, Heck K, Draenert M, Kaisarly D. Current strategies to control recurrent and residual caries with resin composite restorations: operator- and material-related factors. J Clin Med. 2022 Nov 7;11(21):6591. doi: 10.3390/jcm11216591.
Moncada GC, Martin J, Fernandez E, Vildosola PG, Caamano C, Caro MJ, Mjor IA, Gordan VV. Alternative treatments for resin-based composite andamalgam restorations with marginal defects: a 12-month clinical trial. Gen Dent. 2006;54(5):314-318.
Mjor IA. Clinical diagnosis of recurrent caries. J Am Dent Assoc. 2006;136(10):1426-1433. doi: 10.14219/jada.archive.2005.0057.
Mjor IA, Gordan VV. Failure, repair, refurbishing and longevity of restorations. Oper Dent. 2002;27(5):528-534.
Ghulam OA, Fadel HT. Can clusters based on caries experience and medical status explain the distribution of overhanging dental restorations and recurrent caries? A cross-sectional study in Madinah – Saudi Arabia. Saudi J Biol Sci. 2018 Feb;25(2):367-371. doi: 10.1016/j.sjbs.2017.02.001.